Hi friend,
I asked 25 mental health leaders for their 2026 predictions1 .
In today’s article, I combine their insights with my own and share 13 predictions for the mental health market in 2026.
Let’s get into it.
Join The Hemingway Community
We just crossed 290 members. Which is pretty cool. We’ve got big plans for 2026 including local Chapters (with local events), lots of online expert sessions, operator and market guides and much more. It’s a high-quality, diverse group of other mental health nerds AND, today is the last day in 2025 that I will add new members. So join now. It’s only $29 / month.
Key Takeaways
Don’t have time to read the full report? No worries, here are my 13 predictions:
General-Purpose LLMs Become a Major Source of Referrals
Therapy Growth Slows
Population Specific Solutions Steal Share From Larger Platforms
The Big Exit Finally Arrives (we get a mental health IPO)
Consolidation Intensifies (more M&A)
The Clinician Experience Is Reshaped by AI
Medication Sees Increased Client Pushback
Business Pivot From a Story About Access to A Story About Quality
Mental Health UX Gets a Major Upgrade (driven by AI)
Regulatory Frameworks Crystallise, But Evaluation Infrastructure Remains Fragmented
Psychedelics Move from Hype to Healthcare (With at least one treatment getting FDA Approval)
The Negative Impacts of AI Show Up in Therapy Rooms
Consumers Drive Demand for Non-Medicalised Solutions
OK, want to hear more about each of these? Let’s get into them…
1. General-Purpose LLMs Become a Major Source of Referrals
Prediction: ChatGPT, Claude, and other general-purpose AI assistants emerge as a major referral source for mental healthcare.
Everyone is using an LLM. And they’re talking to them about their mental health.
Jackie Ourman, Therapist and Founder of the Social Connection articulated it well: "People are already using general AI tools for emotional support and companionship, and in 2026 that behavior is likely to grow dramatically. Large language models are becoming a place people turn when they feel overwhelmed, lonely, or unsure how to handle the normal challenges of real human relationships."
But the makers of these LLMs don’t want to hold mental health risk.
OpenAI’s recent announcements make that very clear. They are already facing several large lawsuits for the mental health risk they allegedly create. So, they are developing pathways to refer people to professional help. In 2026 millions of people will use these tools to chat about their mental health, and the tools will partner with third parties to refer them out to support. We are already seeing evidence of this through OpenAI’s partnership with Throughline. This dynamic will make general-purpose LLMs a significant referral source for therapy and other mental health services.
2. Therapy Growth Slows
Prediction: The growth in therapy volume will slow in 2026, due to economic and cultural headwinds.
More people than ever are in therapy. For the most part, this is a good thing. Stigma reduction, greater cultural acceptance and increased affordability (driven by insurance coverage) have driven this increase over the last decade. But in 2026, these demand drivers will face challenges.
In 2026, payers will crack down on Behavioural Health expenditure. Their costs have been growing significantly, and many are under financial pressure. They will try to bring these costs down and will pull crude levers to do so. They will lower rates, challenge coverage, and just make it more difficult for members to access therapy. We are already seeing early signs of this.
The cultural narrative around therapy is also starting to shift. Some critics say that within certain demographics, therapy has become less about clinical need and more about lifestyle support, or even more dramatically, a luxury service. Payers do not want to pay for luxury lifestyle services. Some bad therapy businesses have damaged the brand of therapy. I also hear more and more about the “pathologisation of normal human experience”. Whether we believe in these ideas or not, I see them gaining cultural traction and anticipate that they will combine to put downward pressure on the demand side of therapy in 2026.
There will also be more questions around efficacy and ROI. We know that therapy can be an incredible treatment - I’ve mentioned before how much I have personally benefited from therapy - but data on ROI for payers has been sparse. They will ask for more of it in 2026, and if it’s not available, they will use it as a reason to put pressure on therapy providers. Lower rates and poorer coverage from payers will further reduce demand.
Finally, the emergence of low-cost or free alternatives will serve as a final demand-side headwind. Affordability of therapy is a major barrier for consumers. And whether we like it or not, people are now using AI as a source of support. Some will choose that free, always-available service over going to see a therapist. If consumers have less money, the cost of therapy increases, and there’s something free they want to use instead, demand for therapy will reduce.
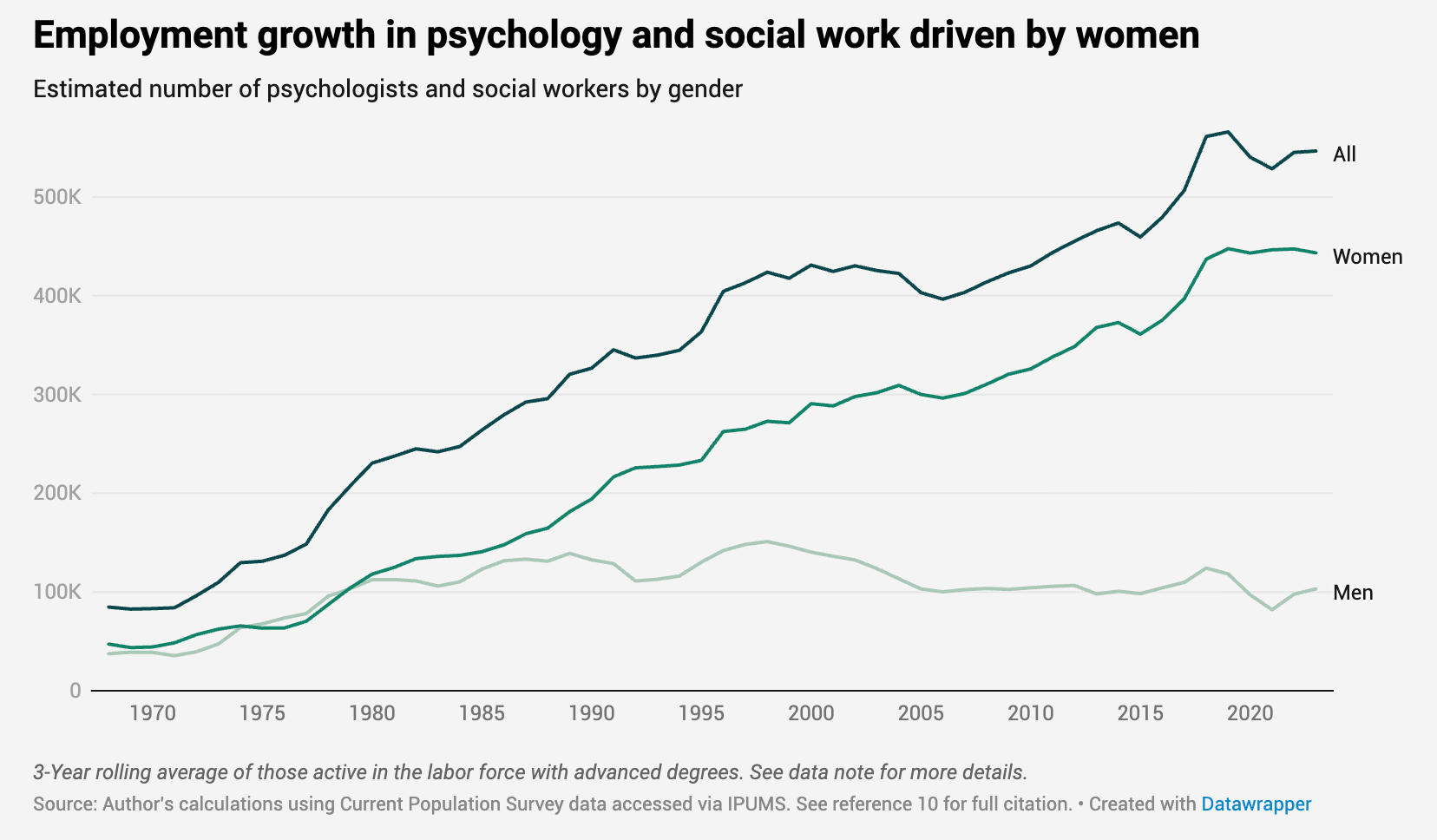
I had originally considered whether this prediction might be “The US reaches peak therapy”, but there are still strong drivers on both the demand and supply side. Rates of mental illness and general distress appear to still be rising, and the supply of therapists also still appears to be increasing2 .
Taking all this into account, I don’t think we’ll hit “peak therapy” in 2026, but the rate of growth will slow.
3. Population Specific Solutions Steal Share
Prediction: One-size-fits-all mental health platforms will lose market share to companies built for specific populations.
Large platforms benefit from scale. But they struggle to match companies that design exclusively for one population's specific needs.
Michelle Turner, Founder of Here Now Health explains her experience with this dynamic: "After a year of pitching to investors and health plans, I'm convinced most are tired of broad, one-size-fits-all mental health solutions that claim to serve everyone but feel built for no one. One size fits all care doesn't fail because people are 'hard to engage,' but because broad systems were never designed for the realities of most people's lives."
Virtual care removes traditional constraints that make population-focused care easier. Turner continues: "Without the limits of brick and mortar, we can design systems shaped by real life. If we built a hospital just for teens, what would it look like? One just for middle-aged women? Virtual care lets us do that!"
Examples are proliferating: FamilyWell for women's mental health, Cerula Care for cancer patients, Here Now Health for foster-impacted youth or even Sharp Performance for people in high-risk professions. These companies benefit from easier client acquisition, higher retention and (probably) better outcomes than large platforms.
But there’s another benefit too: these businesses can more easily bring down total healthcare costs for their patient groups. Mental health is often a comorbidity driving medical spending - addressing it in the context of cancer treatment, maternal health, etc., can drive down total medical spending and give these providers a chance to capture some of those benefits from payers.
4. The Big Exit Finally Arrives
Prediction: We see a big mental health tech IPO in 2026
A few mental health tech companies are close to an IPO. In 2026 I think we’ll see at least one go public. They have the size, profitability and growth to tell a compelling story to Wall Street. While they will ideally want some revenue-generating AI products in market before going public, they will probably still be able to spin a narrative around upside potential.
Yes, mental health valuations remain suppressed, but I think this crop of companies has enough differentiation from the existing public mental health companies to argue that they should be valued differently. Whether investors buy that story and whether the IPO window stays open long enough for them to get out, remains to be seen. But I predict we will see at least one mental health tech IPO in 2026.
5. Consolidation Intensifies
Prediction: We see increased consolidation across the ecosystem with more active M&A markets
There are a lot of late-stage mental health companies that won’t find a path to IPO. They haven’t reached scale, might just be breaking even, but even if they are, they can’t raise another round.
With no IPO or capital markets options, they will look to consolidate through M&A. This has already begun in 2025 and will intensify in 2026. Sub-scale players will merge with each other (like Cerebral and Resilience Lab did in 2025). Bigger players will try to buy smaller fish for IP, technical abilities or to expand their service offering (e.g., Talkspace buying Wisdo).
6. The Clinician Experience Is Reshaped by AI
Prediction: AI transforms the day-to-day life of clinicians - beginning to shift them from time-based service delivery to more continuous oversight, clinical judgment, and escalation management.
Saying AI will transform care delivery feels like a cliché. But that doesn’t make it false. My main reason for including this as a prediction for 2026 is that I believe there are a lot of strong forces at play that will make this shift inevitable.
Payers and health systems want increased efficiency. This is why companies like Limbic, Jimini and others, which are unbundling care delivery and automating it with AI, have seen such strong traction.
Lynn Hamilton, Chief Commercial Officer at Jimini Health describes this care transformation: "In 2026, we'll see the clinician role increasingly emphasize oversight, personalization, and escalation, supported by tools that help patients engage day-to-day. That structure works best when it's built on strong clinical collaboration: clinicians and care teams aligned around shared measurement, consistent care plans, and clear responsibilities for monitoring and follow-up."
If AI is implemented thoughtfully, it has the potential to improve the clinician experience but also to significantly improve client outcomes. Hamilton describes how "mental health outcomes are often driven by what happens between sessions - skill practice, reflection, adherence to plans, early identification of relapse signals, and timely course-correction."
In 2026, most businesses will focus on solving this “between sessions” problem with AI, and it will impact how clinicians work. They will assign homework through AI features, review AI-created notes before sessions, and have responsibility in reviewing the interventions delivered by conversational AI agents. It looks like therapy really is getting unbundled.
Because an increasing number of clinicians are working for large mental health businesses or operating through tech platforms, they may be forced to adopt these new AI tools. That will drive continued change to their role. The important thing is that it is done thoughtfully, safely and with both the client and clinician in mind.
7. Medication Sees Increased Client Pushback
Prediction: More patients and clinicians look for alternatives to medication, and we see a surge of people looking to get off their medication.
Brandon Goode, Co-Founder of Outro Health shared his perspective on this.
"People and clinicians are starting to realize that the models they've been taught aren't actually true (whether partially or completely), and possibly making them feel worse in the long run”
Brandon runs a company that helps people get off psychiatric medication, so I can understand why he has this view. But his view holds up to scrutiny from the evidence. We know that anti-depressants fail to achieve remission for the majority of patients, even when combined with psychotherapy. We also know they can have bad side effects.
“Most people don't know that the majority of diagnosed Major Depressive Disorder naturally goes away (remission) within a year. Time is the best medicine, and using medications for too long can trap you in a cycle. It's not opinion, it's basic science. And it's a huge, overlooked, and misunderstood problem.” Brandon Goode.
Medication is baked deep into the mental healthcare system. And while it most definitely has a place, I think we will see greater patient awareness of its pitfalls and side effects in 2026, leading to more people questioning their treatment. If this happens, companies like Outro will be very helpful in helping patients carefully manage that transition.
8. Business Pivot From a Story About Access to A Story About Quality
Prediction: Mental health businesses will shift their pitch and products to prioritise quality
If you’ve been reading The Hemingway Report for a while, you know that I’ve been harping on about this shift for a while. In 2026, I expect it to continue. Access is not a solved problem. But in 2026, payers will ask more about outcomes and ROI than about access. Companies will respond.
Companies should not just shift their payer messaging, however. They must actually change their service to ruthlessly focus on improving outcomes. They’ll communicate that to their payers, but there’s a huge opportunity to also communicate that to their clients. Who owns the brand position of "highest quality mental healthcare provider?” You know who?? Nobody! And that’s an opportunity.
9. Mental Health UX Gets a Major Upgrade (driven by AI)
Prediction: Patient-driven AI adoption forces the industry to rethink their consumer experience, reshaping how care feels and functions.
Elliot Taylor, Founder of Throughline explains this dynamic well;
“Mental health has always had a user experience problem. People often aren't happy with how hard it is to get support, how much it costs, and the quality of care they receive. The job to be done remains the same: ease of access in a way that feels personal, isn't scary, and actually helps.
AI is transformative not because it's interesting technology, but because it's causing a whole lot of builders to prioritize user experience. In 2026, the biggest impact won't be AI itself, but how AI transforms the user experience.”
Lynn Hamilton from Jimini Health echoes this sentiment: "Patients aren't waiting for the system to approve it - they're already using AI for day-to-day support: journaling, skill practice, problem-solving, and in-the-moment coaching. Patient behavior is a powerful forcing function."
Businesses are reacting to the demands of their clients. For example, in 2025, they all started building chatbots. The forcing function is strong and will continue in 2026.
Adoption of AI into the client journey won’t just improve the user experience, but can significantly improve the quality of care and client outcomes.
Jenna Glover, Chief Clinical Officer at Headspace shared with me how she thinks we can deliver on this.
"AI opens the door to a new depth of personalization that's not just about who someone is, but when they're most open to change. We call this the 'window for change' - a moment when someone's emotions are activated just enough to be receptive to support, but not overwhelmed. That's when AI can deliver the right intervention, at the right time, in the right dose.
Glover also sees significant potential for AI to improve client assessment and diagnosis:
“With the potential to power dynamic, in-the-moment assessment, we could align support with emotional readiness, not just identity or diagnosis. This includes detection through patterns in sleep, usage, mood, and how someone engages with content.”
The user experience and overall outcomes for mental healthcare are due for an upgrade. In 2026, businesses will be forced to deliver on both.
10. Regulatory Frameworks Crystallise But Evaluation Infrastructure Remains Fragmented
Prediction: The FDA delivers clear guidance on how it regulates AI in mental health, and companies will be forced to choose a path. However, the lack of consistent evaluation standards will remain a challenge for the market.
Lisa Palko from the Society for Digital Mental Health shared her thoughts on this:
"The trend I expect to have the biggest impact on the mental health industry in 2026 is regulation. We saw FDA cleared products for major depressive disorder both as an adjunctive and standalone treatment. Reimbursement pathways were created through the Physician Fee Schedule for FDA-cleared products and specified disorders. However, we've also seen the need for clearer regulatory guidance as clinical-grade AI products have been stifled by a regulatory system not fit for purpose."
The FDA have already gathered input on how AI should be regulated in mental health and is expected to clarify its regulations soon. This will close the grey area in which many mental health companies currently operate (acting like therapy, but not actually making therapeutic claims). They will be forced to make a choice to either pursue FDA clearance or stay as a wellness product.
TEMPO (Technology-Enabled Meaningful Patient Outcomes) is the one exception to this path. It will allow a small number of businesses (ten in behavioural health) to commercially deploy their products and charge for them without going through the traditional FDA premarket authorisation process. Combined with ACCESS as a new payment model, this will create a pretty exciting opportunity for digital mental health players.
Lisa Palko explains the significance: "We are most excited about the expansion of large-scale access initiatives such as ACCESS and TEMPO programs. For digital mental health to have a true population-level impact, we need programs that support its use in populations that have traditionally been less likely to receive innovative services. Payment models that emphasize outcomes and value-based care provide opportunities for population-level benefits."
But regulatory clarity doesn't solve the evaluation challenge. Xuan Zhao, Co-Founder of Flourish Science identifies what's missing: "The biggest constraint is the lack of widely recognized third-party assessment, quality assurance, and credentialing standards that distinguish well-designed mental health AI tools from less effective or potentially unsafe ones. Organizations know they need scalable, tech-enabled support, but they struggle to evaluate which solutions are truly evidence-based, clinically informed, and safe."
In the AI space, a few evaluation frameworks have emerged. But none are close to being established as an industry standard. Federal agencies will clarify what's legal. But the market will still struggle to know what works.
11. Psychedelics Move from Hype to Healthcare
Prediction: We will see at least one FDA approval of psychedelic treatments, and continued psychedelics expansion through other access models.
I asked Josh Hardman, Founder of Psychedelic Alpha, what he expects in the market in 2026. Josh knows more than anyone about what is happening in the psychedelics space and always approaches it with intellectual honesty. As a result, I massively respect his opinion. He told me that:
“2026 is going to be a very interesting year for the psychedelics field, not only on the drug development and potential FDA approval front, but also in terms of state access models in the U.S. and developments in Europe and Australia.”
“In the U.S., we will see whether the perceived regulatory tailwinds for the class of drugs translate to concrete developments. I expect to see up to three FDA approvals of psychedelics in the next 18 months, and two of those could come in 2026. But while the political situation appears to be favourable to psychedelics, it’s not clear just how deep that support runs, especially in an election year. While MAHA is broadly ‘pro psychedelics’, MAGA - including ‘young MAGA’ - isn’t so convinced, I hear.”
“Still, the allure of a new treatment option for mental health disorders, especially given interest and demand from Veterans, tips the balance of probability toward some substantive action next year, in my view. Many of us in the field are just hoping that any approval is on the merits of the submission and data.”
While it sounds like we can expect treatments to progress down traditional regulatory pathways, we can also expect psychedelic treatments to start to reach patients in other ways. Josh shed some light on this for me:
“Outside of the traditional marketing authorisation model, some U.S states and other countries are setting up alternative psychedelics access models. In 2026, we expect to see the first legal medical psilocybin administered in Czechia, Germany’s psilocybin compassionate use program should get underway in earnest, and Australia’s psychedelics program should continue to grow. In the U.S., New Mexico’s Medical Psilocybin program could get off the ground in very late 2026, and Colorado’s ‘natural medicine’ (psychedelics) program should also begin to grow. I also expect lots of states to introduce Bills to their legislatures in the first months of 2026, which will seek things like funding for psychedelic research, pilot programs, state-legal psychedelic access programs, and regulatory tweaks around the drugs’ use in research or medical practice.”
I’ve been looking at psychedelics with tempered optimism for a while, but it looks like 2026 will be a year of progress, increased access and greater real-world experimentation for the field.
12. The Negative Impacts of AI Show Up in Therapy Rooms
Prediction: Clinicians see a significant increase in AI-induced mental health conditions
Coley Williams, Senior Director of Mental Health at First Stop Health, identified what he sees coming:
"Much like every other major societal shift, AI won't just change how we get care - it will change what we need care for. We will increasingly see themes like: Loss of meaning or confidence as AI automates familiar tasks, strain on interpersonal dynamics ('Why ask my partner when I can just ask AI?'), anxiety about relevance, surveillance, or job stability, identity shifts related to creativity, productivity, and self-worth, over-reliance on AI as a pseudo-attachment figure or decision-maker."
Jackie Ourman sees the attachment issues emerging: "For those who struggle with conflict, shame, or insecure attachment, AI can feel like a 'perfect listener' where they never risk being misunderstood or challenged. Instead of helping people build healthier relationships, it can reinforce avoidance, deepen isolation, and create emotional dependence on something incapable of responding in a human way."
On top of these concerns, I am particularly worried about AI companions. They are widespread, powerful and have the potential to cause significant harm. While social media fights for our attention, AI Companions fight for our attachment. I didn’t think there could be a more concerning mass technology than social media, and yet, here we are…
Although ethical standards and regulation are coming to this space, they are slow. In the meantime, the depth and breadth of this technology will cause significant disruption in our lives, and that will show up in the therapy room.
Ourman sums it up well: "The mental health field is not prepared for this scale of reliance. We are likely to see harm before ethical standards catch up."
13. Consumers Drive Demand for Non-Medicalised Solutions
Prediction: We see a significant increase in the adoption of non-clinical interventions for mental health.
There are truths so fundamental that we often fail to give them the attention they deserve. I believe the impact of our social and environmental circumstances on our mental health is one of those truths.
Carmine Di Maro, Executive Director at One Mind frames the opportunity: "I think we need to address some of the root causes of mental health challenges - social determinants of health, access to social connection, nature, arts, diet and physical activity, gaps in income, access to resources like transportation and support networks - and make evidence-based versions of these things accessible to people at scale."
Carmine is right. In 2026, I believe policymakers and clinicians will increasingly adopt this approach. But perhaps more importantly, so will individuals. People know that social connection, exercise, sleep and other non-medical interventions make them feel better. It’s both logical and intuitive. As people look for ways to improve their own mental health in 2026, they will seek out more of these kinds of services. We are already seeing evidence of this in the growth of wellness retreats, social clubs, run clubs, sleep products and more.
We may also see these non-medical interventions increasingly recommended by clinicians.
Chris Appleton from SocialRx (Art Pharmacy) sees momentum building: "The idea I am most excited about is the rapid expansion of social prescribing as a core component of population mental health. Social prescribing recognizes that well-being is shaped as much by connection and community as by traditional clinical care. In 2026 I see growing interest from employers, health plans and public agencies that want new approaches to support mental well-being at scale."
Non-medicalised interventions are cheap, facilitate early intervention, and address root causes rather than symptoms. This approach is aligned with Sondermind VP Val Young’s main hope for 2026: that we deepen the connection between our physical and mental health.
“[my hope is for us] all to understand the interconnectivity of sleep, stress, movement & nutrition on our mental health. And to treat each of those as a proactive, preventative actions (vs reactive) to maintain and improve population mental health.”
Payers and individuals are looking for alternative ways to improve mental health. Clever provider organisations will find ways to make that happen with non-medical interventions.
OK, those are my 13 predictions for 2026. Do you agree? Have I missed something? Reach out and let me know. I’m setting a reminder to check back in twelve months and see how I did.
That’s all for this week. And that’s all for this year! Thank you so much for reading these reports and supporting my work. Have a great holiday period and remember…
Keep fighting the good fight!
Steve
Founder of Hemingway
[1] Many thanks to everyone who contributed their insights. If you weren’t referenced in this report directly, apologies; it was a difficult challenge to edit and synthesise all responses. I also gathered feedback on the major challenges these leaders are facing and will share those insights in a separate report in the new year.
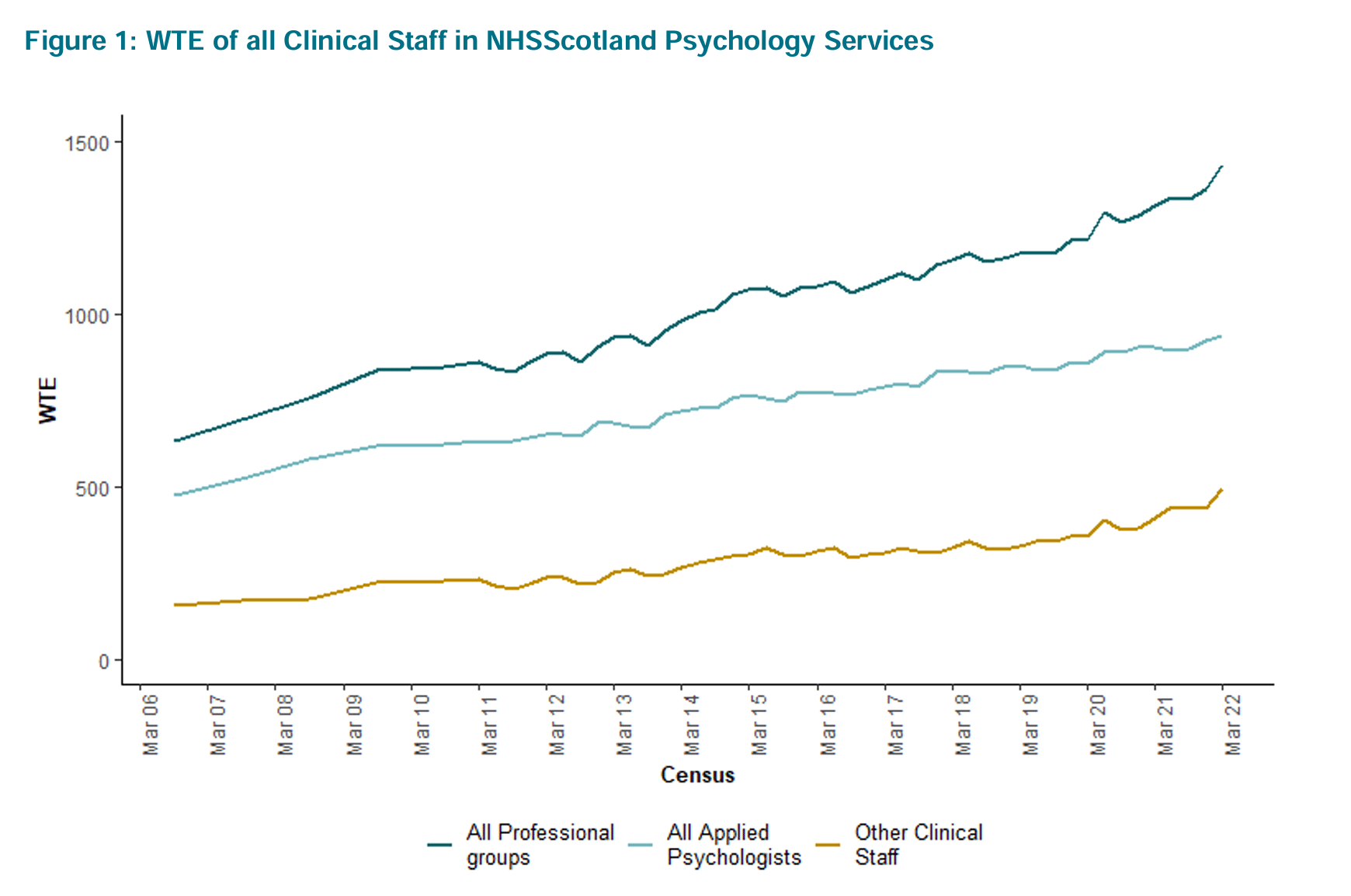
[2] I’ve found it incredibly hard to get good data on the mental health workforce supply in the US. The graphs below seem to show annual workforce growth somewhere between 5% and 10%. But the datasets end in 2022, meaning we don’t know if this growth has continued through to 2025. If you know of good datasets that can help me answer this question, please send them my way.